-
4 Berichten
-
1 foto's
-
0 Video’s
-
Woont in Surat
-
Vanaf Surat
-
Female
-
07/06/1991
-
Gevolgd door 0 people
Actueel
-
How Pelvic Floor Exercises Can Help with Overactive Bladder
Overactive bladder (OAB) is a condition that affects millions of people worldwide, causing a frequent and urgent need to urinate. While medications and lifestyle changes are often prescribed, pelvic floor exercises, also known as Kegel exercises, can play a significant role in managing OAB symptoms naturally. These exercises strengthen the muscles that control urination, offering relief to those struggling with overactive bladder, neurogenic bladder, and other related conditions, such as neurogenic bladder due to meningomyelocele.
Understanding Overactive Bladder and Neurogenic Bladder
Overactive bladder refers to a condition where the bladder muscles contract involuntarily, causing a sudden and intense urge to urinate. In contrast, a neurogenic bladder is typically caused by neurological disorders or damage to the nervous system, such as spinal cord injuries, stroke, or conditions like meningomyelocele. Neurogenic bladder often results in the inability to control urination, leading to leakage or retention.
In both cases, weakened pelvic floor muscles can exacerbate symptoms. Strengthening these muscles through regular exercises can improve bladder control and reduce symptoms of both OAB and neurogenic bladder.
How Pelvic Floor Exercises Work
Pelvic floor exercises target the muscles that support the bladder, uterus, and bowel. These muscles play a crucial role in controlling urine flow. When they are weak, they are unable to function properly, leading to issues like urinary incontinence, a key symptom of overactive bladder.
By regularly performing pelvic floor exercises, individuals can:
Improve Bladder Control: Stronger pelvic muscles help reduce involuntary bladder contractions, which are the primary cause of frequent urination in OAB.
Reduce Urine Leakage: With neurogenic bladder conditions, strengthening the pelvic muscles can minimize urine leakage, providing more control over urination.
Enhance Muscle Tone: For individuals with neurogenic bladder due to meningomyelocele, pelvic floor exercises help maintain muscle tone, improving bladder function even when neurological control is compromised.
How to Perform Pelvic Floor Exercises
Pelvic floor exercises are simple and can be done almost anywhere. Here’s a quick guide:
Identify the Muscles: The easiest way to identify your pelvic floor muscles is by trying to stop the flow of urine midstream. The muscles you use to do this are your pelvic floor muscles.
Contract and Hold: Once you’ve identified the muscles, contract them for five seconds, then relax for five seconds. Gradually work up to holding the contraction for 10 seconds at a time.
Repeat: Aim to complete 10 to 15 repetitions, three times a day. Consistency is key to seeing results.
Benefits for Neurogenic Bladder Due to Meningomyelocele
Meningomyelocele, a birth defect where the spinal cord does not develop properly, often leads to neurogenic bladder. Individuals with this condition may experience difficulty in controlling bladder function. While pelvic floor exercises cannot cure the neurological damage, they can help manage symptoms by providing better muscle support to the bladder, enhancing quality of life.
Conclusion
Pelvic floor exercises offer a non-invasive, natural way to manage symptoms of overactive bladder and neurogenic bladder, including conditions stemming from meningomyelocele. When performed consistently, these exercises can strengthen the pelvic muscles, reduce leakage, and improve bladder control. For more information on managing bladder issues and other urological conditions, visit Subodh Urology, a comprehensive resource for expert care and treatment options.
Read More - https://subodh-urology.com/overactive-bladder/
How Pelvic Floor Exercises Can Help with Overactive Bladder Overactive bladder (OAB) is a condition that affects millions of people worldwide, causing a frequent and urgent need to urinate. While medications and lifestyle changes are often prescribed, pelvic floor exercises, also known as Kegel exercises, can play a significant role in managing OAB symptoms naturally. These exercises strengthen the muscles that control urination, offering relief to those struggling with overactive bladder, neurogenic bladder, and other related conditions, such as neurogenic bladder due to meningomyelocele. Understanding Overactive Bladder and Neurogenic Bladder Overactive bladder refers to a condition where the bladder muscles contract involuntarily, causing a sudden and intense urge to urinate. In contrast, a neurogenic bladder is typically caused by neurological disorders or damage to the nervous system, such as spinal cord injuries, stroke, or conditions like meningomyelocele. Neurogenic bladder often results in the inability to control urination, leading to leakage or retention. In both cases, weakened pelvic floor muscles can exacerbate symptoms. Strengthening these muscles through regular exercises can improve bladder control and reduce symptoms of both OAB and neurogenic bladder. How Pelvic Floor Exercises Work Pelvic floor exercises target the muscles that support the bladder, uterus, and bowel. These muscles play a crucial role in controlling urine flow. When they are weak, they are unable to function properly, leading to issues like urinary incontinence, a key symptom of overactive bladder. By regularly performing pelvic floor exercises, individuals can: Improve Bladder Control: Stronger pelvic muscles help reduce involuntary bladder contractions, which are the primary cause of frequent urination in OAB. Reduce Urine Leakage: With neurogenic bladder conditions, strengthening the pelvic muscles can minimize urine leakage, providing more control over urination. Enhance Muscle Tone: For individuals with neurogenic bladder due to meningomyelocele, pelvic floor exercises help maintain muscle tone, improving bladder function even when neurological control is compromised. How to Perform Pelvic Floor Exercises Pelvic floor exercises are simple and can be done almost anywhere. Here’s a quick guide: Identify the Muscles: The easiest way to identify your pelvic floor muscles is by trying to stop the flow of urine midstream. The muscles you use to do this are your pelvic floor muscles. Contract and Hold: Once you’ve identified the muscles, contract them for five seconds, then relax for five seconds. Gradually work up to holding the contraction for 10 seconds at a time. Repeat: Aim to complete 10 to 15 repetitions, three times a day. Consistency is key to seeing results. Benefits for Neurogenic Bladder Due to Meningomyelocele Meningomyelocele, a birth defect where the spinal cord does not develop properly, often leads to neurogenic bladder. Individuals with this condition may experience difficulty in controlling bladder function. While pelvic floor exercises cannot cure the neurological damage, they can help manage symptoms by providing better muscle support to the bladder, enhancing quality of life. Conclusion Pelvic floor exercises offer a non-invasive, natural way to manage symptoms of overactive bladder and neurogenic bladder, including conditions stemming from meningomyelocele. When performed consistently, these exercises can strengthen the pelvic muscles, reduce leakage, and improve bladder control. For more information on managing bladder issues and other urological conditions, visit Subodh Urology, a comprehensive resource for expert care and treatment options. Read More - https://subodh-urology.com/overactive-bladder/0 Reacties 0 aandelen 53 Views 0 voorbeeldPlease log in to like, share and comment! -
Neurogenic Bladder and Quality of Life: Strategies for Better Daily Living
Neurogenic bladder, a condition arising from nerve damage, disrupts bladder control and function, posing significant challenges to daily life. It can result from spinal cord injuries, neurological disorders, or congenital conditions such as meningomyelocele. Despite these difficulties, effective management and lifestyle adjustments can significantly enhance quality of life. This article explores strategies for managing neurogenic bladder and improving daily living.
Understanding Neurogenic Bladder
Neurogenic bladder occurs when communication between the brain and bladder is impaired due to nerve damage. In conditions like meningomyelocele—a congenital defect of the spinal cord—this disruption leads to bladder dysfunction. Depending on the severity of the nerve damage, patients may experience:
Overactive Bladder (OAB): Characterized by frequent urges to urinate and possible incontinence.
Underactive Bladder: Difficulty emptying the bladder fully, resulting in discomfort and urinary retention.
Challenges and Impact on Quality of Life
Living with neurogenic bladder can be emotionally and physically taxing. Unpredictable bladder function often interferes with daily activities, social engagements, and mental health. Many individuals avoid social interactions or physical activities due to fear of incontinence or frequent bathroom trips. However, there are actionable strategies to address these challenges and improve overall well-being.
Strategies to Improve Daily Living
Medical Treatments
Working with a healthcare provider is essential for effective management. Treatment plans may include:
Medications: To manage symptoms like urgency and frequency in OAB.
Catheterization: For underactive bladder cases to ensure proper emptying.
Surgical Interventions: In severe cases, procedures like bladder augmentation or reconstruction can restore function.
Pelvic Floor Strengthening
Performing pelvic floor exercises, such as Kegels, can improve bladder control by strengthening the muscles that regulate urination. Consistent practice can reduce incontinence episodes and enhance confidence.
Dietary Modifications
Nutrition plays a critical role in bladder health. To minimize irritation:
Avoid bladder irritants like caffeine, alcohol, and spicy foods.
Stay hydrated with water, but monitor fluid intake, particularly in the evening, to reduce nighttime disruptions.
Bladder Training
Gradually increasing the interval between bathroom visits can retrain the bladder to hold more urine and reduce urgency. This technique is especially useful for those managing OAB symptoms.
Support Systems and Tools
Specialist Care: Consulting with a urologist ensures personalized care and access to the latest treatments. Specialists, such as those at Subodh Urology, offer tailored support for neurogenic bladder management.
Assistive Devices: Catheter systems, incontinence pads, or other discreet tools can help manage symptoms effectively, allowing for greater confidence in social and professional settings.
Conclusion
Neurogenic bladder, including cases caused by conditions like meningomyelocele, presents unique challenges. However, with the right combination of medical care, lifestyle changes, and supportive tools, individuals can significantly improve their quality of life. Proactive management fosters independence and restores confidence, enabling people to lead fulfilling lives.
For expert guidance and advanced treatment options for neurogenic bladder, visit Subodh Urology, where dedicated professionals provide comprehensive and compassionate care tailored to your needs.
Read More - https://subodh-urology.com/functional-urology-female-urology-neuro-urology/
Neurogenic Bladder and Quality of Life: Strategies for Better Daily Living Neurogenic bladder, a condition arising from nerve damage, disrupts bladder control and function, posing significant challenges to daily life. It can result from spinal cord injuries, neurological disorders, or congenital conditions such as meningomyelocele. Despite these difficulties, effective management and lifestyle adjustments can significantly enhance quality of life. This article explores strategies for managing neurogenic bladder and improving daily living. Understanding Neurogenic Bladder Neurogenic bladder occurs when communication between the brain and bladder is impaired due to nerve damage. In conditions like meningomyelocele—a congenital defect of the spinal cord—this disruption leads to bladder dysfunction. Depending on the severity of the nerve damage, patients may experience: Overactive Bladder (OAB): Characterized by frequent urges to urinate and possible incontinence. Underactive Bladder: Difficulty emptying the bladder fully, resulting in discomfort and urinary retention. Challenges and Impact on Quality of Life Living with neurogenic bladder can be emotionally and physically taxing. Unpredictable bladder function often interferes with daily activities, social engagements, and mental health. Many individuals avoid social interactions or physical activities due to fear of incontinence or frequent bathroom trips. However, there are actionable strategies to address these challenges and improve overall well-being. Strategies to Improve Daily Living Medical Treatments Working with a healthcare provider is essential for effective management. Treatment plans may include: Medications: To manage symptoms like urgency and frequency in OAB. Catheterization: For underactive bladder cases to ensure proper emptying. Surgical Interventions: In severe cases, procedures like bladder augmentation or reconstruction can restore function. Pelvic Floor Strengthening Performing pelvic floor exercises, such as Kegels, can improve bladder control by strengthening the muscles that regulate urination. Consistent practice can reduce incontinence episodes and enhance confidence. Dietary Modifications Nutrition plays a critical role in bladder health. To minimize irritation: Avoid bladder irritants like caffeine, alcohol, and spicy foods. Stay hydrated with water, but monitor fluid intake, particularly in the evening, to reduce nighttime disruptions. Bladder Training Gradually increasing the interval between bathroom visits can retrain the bladder to hold more urine and reduce urgency. This technique is especially useful for those managing OAB symptoms. Support Systems and Tools Specialist Care: Consulting with a urologist ensures personalized care and access to the latest treatments. Specialists, such as those at Subodh Urology, offer tailored support for neurogenic bladder management. Assistive Devices: Catheter systems, incontinence pads, or other discreet tools can help manage symptoms effectively, allowing for greater confidence in social and professional settings. Conclusion Neurogenic bladder, including cases caused by conditions like meningomyelocele, presents unique challenges. However, with the right combination of medical care, lifestyle changes, and supportive tools, individuals can significantly improve their quality of life. Proactive management fosters independence and restores confidence, enabling people to lead fulfilling lives. For expert guidance and advanced treatment options for neurogenic bladder, visit Subodh Urology, where dedicated professionals provide comprehensive and compassionate care tailored to your needs. Read More - https://subodh-urology.com/functional-urology-female-urology-neuro-urology/0 Reacties 0 aandelen 76 Views 0 voorbeeld -
Lifestyle Changes to Manage an Overactive Bladder
Dealing with an overactive bladder (OAB) can be frustrating, but with the right lifestyle changes, it is possible to manage the symptoms effectively. Overacting bladder is a condition characterized by a sudden urge to urinate, sometimes leading to involuntary leakage. While this condition can impact daily life, simple adjustments can help improve bladder control and reduce the frequency of bathroom trips.
1. Dietary Adjustments
Certain foods and beverages are known to irritate the bladder and exacerbate symptoms of overacting bladder. Cutting down on caffeine, alcohol, carbonated drinks, and spicy foods can reduce bladder irritation. Instead, focus on a diet rich in fiber, as constipation can worsen bladder problems. Staying hydrated is also important, but moderation is key. Drinking too much fluid can increase urine output, while too little can concentrate urine and irritate the bladder lining.
2. Timed Voiding
Timed voiding, or bladder training, involves scheduling bathroom visits at regular intervals instead of waiting for the urge to strike. This technique helps retrain the bladder to hold more urine and reduces the sudden need to urinate. Start by visiting the bathroom every two hours and gradually increase the time between visits as your bladder adapts.
3. Pelvic Floor Exercises
Strengthening the pelvic floor muscles can provide better control over the bladder. Kegel exercises, which involve tightening and relaxing the pelvic muscles, are particularly effective. By doing these exercises regularly, people with overacting bladder can improve their muscle strength and reduce the likelihood of leakage. It’s important to consult a healthcare professional for guidance on the correct technique.
4. Weight Management
Excess weight puts additional pressure on the bladder, which can worsen overacting bladder symptoms. Maintaining a healthy weight through regular exercise and a balanced diet can alleviate this pressure and improve bladder function. Simple exercises such as walking, swimming, or yoga can help achieve and maintain a healthy weight without straining the bladder.
5. Quit Smoking
Smoking is not only harmful to the lungs but also to bladder health. Smoking can lead to chronic coughing, which weakens the pelvic muscles over time and increases the risk of bladder control issues. Quitting smoking can reduce the frequency of overacting bladder episodes and improve overall health.
6. Managing Neurogenic Bladder
In some cases, overacting bladder may be linked to a condition known as neurogenic bladder, which affects bladder control due to nerve damage. This can be a result of conditions like myelomeningocele, a congenital spinal cord defect. People with neurogenic bladder often require specialized treatment and lifestyle adjustments, such as catheterization, to manage bladder function.
If you are experiencing symptoms related to neurogenic bladder due to myelomeningocele or other neurological conditions, consulting a urologist can help you explore tailored treatment options. For more information, you can visit Subodh Urology, where experts provide specialized care for overacting bladder and neurogenic bladder conditions.
Conclusion
Managing an overacting bladder involves a combination of lifestyle changes and, in some cases, medical interventions. By making small but significant adjustments in diet, exercise, and daily habits, individuals can reduce the frequency of symptoms and improve their quality of life. For those with more complex conditions such as neurogenic bladder, consulting a specialist is essential for effective management and treatment.
Read More - https://subodh-urology.com/overactive-bladder/Lifestyle Changes to Manage an Overactive Bladder Dealing with an overactive bladder (OAB) can be frustrating, but with the right lifestyle changes, it is possible to manage the symptoms effectively. Overacting bladder is a condition characterized by a sudden urge to urinate, sometimes leading to involuntary leakage. While this condition can impact daily life, simple adjustments can help improve bladder control and reduce the frequency of bathroom trips. 1. Dietary Adjustments Certain foods and beverages are known to irritate the bladder and exacerbate symptoms of overacting bladder. Cutting down on caffeine, alcohol, carbonated drinks, and spicy foods can reduce bladder irritation. Instead, focus on a diet rich in fiber, as constipation can worsen bladder problems. Staying hydrated is also important, but moderation is key. Drinking too much fluid can increase urine output, while too little can concentrate urine and irritate the bladder lining. 2. Timed Voiding Timed voiding, or bladder training, involves scheduling bathroom visits at regular intervals instead of waiting for the urge to strike. This technique helps retrain the bladder to hold more urine and reduces the sudden need to urinate. Start by visiting the bathroom every two hours and gradually increase the time between visits as your bladder adapts. 3. Pelvic Floor Exercises Strengthening the pelvic floor muscles can provide better control over the bladder. Kegel exercises, which involve tightening and relaxing the pelvic muscles, are particularly effective. By doing these exercises regularly, people with overacting bladder can improve their muscle strength and reduce the likelihood of leakage. It’s important to consult a healthcare professional for guidance on the correct technique. 4. Weight Management Excess weight puts additional pressure on the bladder, which can worsen overacting bladder symptoms. Maintaining a healthy weight through regular exercise and a balanced diet can alleviate this pressure and improve bladder function. Simple exercises such as walking, swimming, or yoga can help achieve and maintain a healthy weight without straining the bladder. 5. Quit Smoking Smoking is not only harmful to the lungs but also to bladder health. Smoking can lead to chronic coughing, which weakens the pelvic muscles over time and increases the risk of bladder control issues. Quitting smoking can reduce the frequency of overacting bladder episodes and improve overall health. 6. Managing Neurogenic Bladder In some cases, overacting bladder may be linked to a condition known as neurogenic bladder, which affects bladder control due to nerve damage. This can be a result of conditions like myelomeningocele, a congenital spinal cord defect. People with neurogenic bladder often require specialized treatment and lifestyle adjustments, such as catheterization, to manage bladder function. If you are experiencing symptoms related to neurogenic bladder due to myelomeningocele or other neurological conditions, consulting a urologist can help you explore tailored treatment options. For more information, you can visit Subodh Urology, where experts provide specialized care for overacting bladder and neurogenic bladder conditions. Conclusion Managing an overacting bladder involves a combination of lifestyle changes and, in some cases, medical interventions. By making small but significant adjustments in diet, exercise, and daily habits, individuals can reduce the frequency of symptoms and improve their quality of life. For those with more complex conditions such as neurogenic bladder, consulting a specialist is essential for effective management and treatment. Read More - https://subodh-urology.com/overactive-bladder/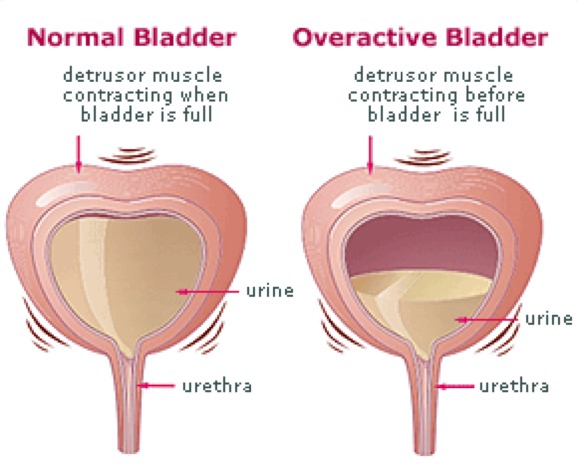 SUBODH-UROLOGY.COMOveractive BladderIf you are experiencing symptoms of overactive bladder and seeking help, we are here to assist you.0 Reacties 0 aandelen 88 Views 0 voorbeeld
SUBODH-UROLOGY.COMOveractive BladderIf you are experiencing symptoms of overactive bladder and seeking help, we are here to assist you.0 Reacties 0 aandelen 88 Views 0 voorbeeld -
0 Reacties 0 aandelen 16 Views 0 voorbeeld
Meer blogs











